The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro
1. Introduction
Ivermectin is an FDA-approved broad spectrum anti-parasitic agent (Gonzalez Canga et al., 2008) that in recent years we, along with other groups, have shown to have anti-viral activity against a broad range of viruses (Gotz et al., 2016; Lundberg et al., 2013; Tay et al., 2013; Wagstaff et al., 2012) in vitro. Originally identified as an inhibitor of interaction between the human immunodeficiency virus-1 (HIV-1) integrase protein (IN) and the importin (IMP) α/β1 heterodimer responsible for IN nuclear import (Wagstaff et al., 2011), Ivermectin has since been confirmed to inhibit IN nuclear import and HIV-1 replication (Wagstaff et al., 2012). Other actions of ivermectin have been reported (Mastrangelo et al., 2012), but ivermectin has been shown to inhibit nuclear import of host (eg. (Kosyna et al., 2015; van der Watt et al., 2016)) and viral proteins, including simian virus SV40 large tumour antigen (T-ag) and dengue virus (DENV) non-structural protein 5 (Wagstaff et al., 2012, Wagstaff et al., 2011). Importantly, it has been demonstrated to limit infection by RNA viruses such as DENV 1-4 (Tay et al., 2013), West Nile Virus (Yang et al., 2020), Venezuelan equine encephalitis virus (VEEV) (Lundberg et al., 2013) and influenza (Gotz et al., 2016), with this broad spectrum activity believed to be due to the reliance by many different RNA viruses on IMPα/β1 during infection (Caly et al., 2012; Jans et al., 2019). Ivermectin has similarly been shown to be effective against the DNA virus pseudorabies virus (PRV) both in vitro and in vivo, with ivermectin treatment shown to increase survival in PRV-infected mice (Lv et al., 2018). Efficacy was not observed for ivermectin against Zika virus (ZIKV) in mice, but the authors acknowledged that study limitations justified re-evaluation of ivermectin's anti-ZIKV activity (Ketkar et al., 2019). Finally, ivermectin was the focus of a phase III clinical trial in Thailand in 2014–2017, against DENV infection, in which a single daily oral dose was observed to be safe and resulted in a significant reduction in serum levels of viral NS1 protein, but no change in viremia or clinical benefit was observed (see below) (Yamasmith et al., 2018).
The causative agent of the current COVID-19 pandemic, SARS-CoV-2, is a single stranded positive sense RNA virus that is closely related to severe acute respiratory syndrome coronavirus (SARS-CoV). Studies on SARS-CoV proteins have revealed a potential role for IMPα/β1 during infection in signal-dependent nucleocytoplasmic shutting of the SARS-CoV Nucleocapsid protein (Rowland et al., 2005; Timani et al., 2005; Wulan et al., 2015), that may impact host cell division (Hiscox et al., 2001; Wurm et al., 2001). In addition, the SARS-CoV accessory protein ORF6 has been shown to antagonize the antiviral activity of the STAT1 transcription factor by sequestering IMPα/β1 on the rough ER/Golgi membrane (Frieman et al., 2007). Taken together, these reports suggested that ivermectin's nuclear transport inhibitory activity may be effective against SARS-CoV-2.
To test the antiviral activity of ivermectin towards SARS-CoV-2, we infected Vero/hSLAM cells with SARS-CoV-2 isolate Australia/VIC01/2020 at an MOI of 0.1 for 2 h, followed by the addition of 5 μM ivermectin. Supernatant and cell pellets were harvested at days 0–3 and analysed by RT-PCR for the replication of SARS-CoV-2 RNA (Fig. 1A/B). At 24 h, there was a 93% reduction in viral RNA present in the supernatant (indicative of released virions) of samples treated with ivermectin compared to the vehicle DMSO. Similarly a 99.8% reduction in cell-associated viral RNA (indicative of unreleased and unpackaged virions) was observed with ivermectin treatment. By 48 h this effect increased to an ~5000-fold reduction of viral RNA in ivermectin-treated compared to control samples, indicating that ivermectin treatment resulted in the effective loss of essentially all viral material by 48 h. Consistent with this idea, no further reduction in viral RNA was observed at 72 h. As we have observed previously (Lundberg et al., 2013; Tay et al., 2013; Wagstaff et al., 2012), no toxicity of ivermectin was observed at any of the timepoints tested, in either the sample wells or in parallel tested drug alone samples.
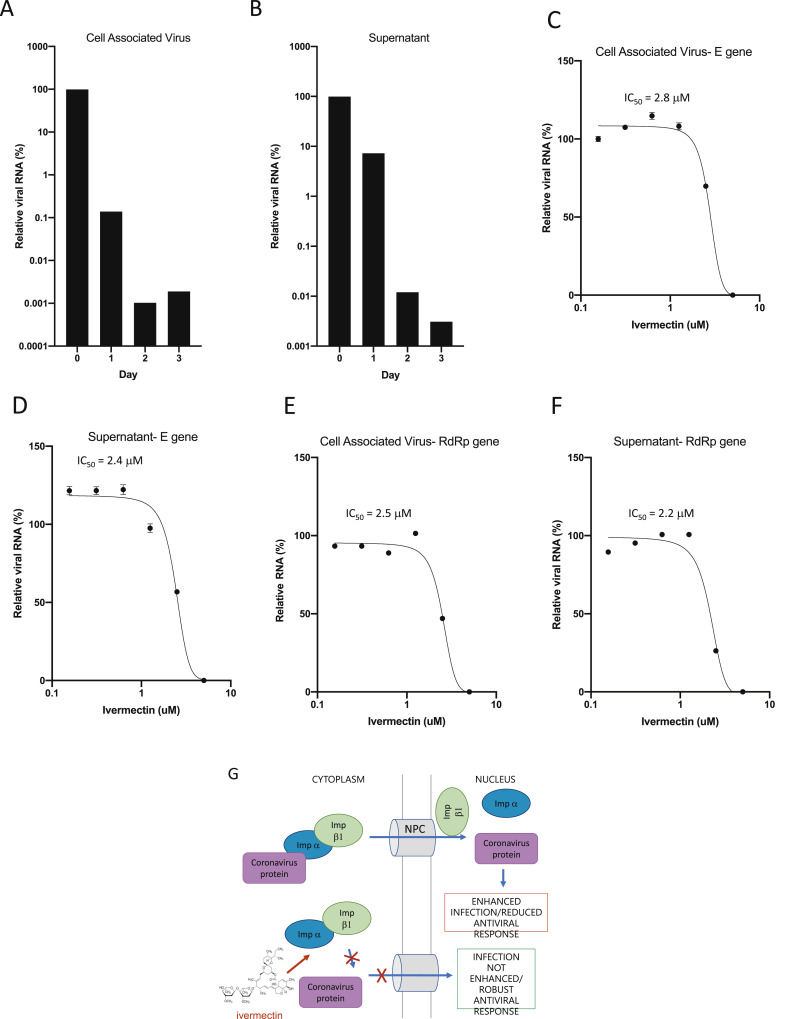
Fig. 1. Ivermectin is a potent inhibitor of the SARS-CoV-2 clinical isolate Australia/VIC01/2020. Vero/hSLAM cells were in infected with SARS-CoV-2 clinical isolate Australia/VIC01/2020 (MOI = 0.1) for 2 h prior to addition of vehicle (DMSO) or Ivermectin at the indicated concentrations. Samples were taken at 0–3 days post infection for quantitation of viral load using real-time PCR of cell associated virus (A) or supernatant (B). IC50 values were determined in subsequent experiments at 48 h post infection using the indicated concentrations of Ivermectin (treated at 2 h post infection as per A/B). Triplicate real-time PCR analysis was performed on cell associated virus (C/E) or supernatant (D/F) using probes against either the SARS-CoV-2 E (C/D) or RdRp (E/F) genes. Results represent mean ± SD (n = 3). 3 parameter dose response curves were fitted using GraphPad prism to determine IC50 values (indicated). G. Schematic of ivermectin's proposed antiviral action on coronavirus. IMPα/β1 binds to the coronavirus cargo protein in the cytoplasm (top) and translocates it through the nuclear pore complex (NPC) into the nucleus where the complex falls apart and the viral cargo can reduce the host cell's antiviral response, leading to enhanced infection. Ivermectin binds to and destabilises the Impα/β1 heterodimer thereby preventing Impα/β1 from binding to the viral protein (bottom) and preventing it from entering the nucleus. This likely results in reduced inhibition of the antiviral responses, leading to a normal, more efficient antiviral response.
To further determine the effectiveness of ivemectin, cells infected with SARS-CoV-2 were treated with serial dilutions of ivermectin 2 h post infection and supernatant and cell pellets collected for real-time RT-PCR at 48 h (Fig. 1C/D). As above, a >5000 reduction in viral RNA was observed in both supernatant and cell pellets from samples treated with 5 μM ivermectin at 48 h, equating to a 99.98% reduction in viral RNA in these samples. Again, no toxicity was observed with ivermectin at any of the concentrations tested. The IC50 of ivermectin treatment was determined to be ~2 μM under these conditions. Underlining the fact that the assay indeed specifically detected SARS-CoV-2, RT-PCR experiments were repeated using primers specific for the viral RdRp gene (Fig. 1E/F) rather than the E gene (above), with nearly identical results observed for both released (supernatant) and cell-associated virus.
Taken together these results demonstrate that ivermectin has antiviral action against the SARS-CoV-2 clinical isolate in vitro, with a single dose able to control viral replication within 24–48 h in our system. We hypothesise that this is likely through inhibiting IMPα/β1-mediated nuclear import of viral proteins (Fig. 1G), as shown for other RNA viruses (Tay et al., 2013; Wagstaff et al., 2012; Yang et al., 2020); confirmation of this mechanism in the case of SARS-CoV-2, and identification of the specific SARS-CoV-2 and/or host component(s) impacted (see (Yang et al., 2020)) is an important focus future work in this laboratory. Ultimately, development of an effective anti-viral for SARS-CoV-2, if given to patients early in infection, could help to limit the viral load, prevent severe disease progression and limit person-person transmission. Benchmarking testing of ivermectin against other potential antivirals for SARS-CoV-2 with alternative mechanisms of action (Dong et al., 2020; Elfiky, 2020; Gordon et al., 2020; Li and De Clercq, 2020; Wang et al., 2020) would thus be important as soon as practicable. This Brief Report raises the possibility that ivermectin could be a useful antiviral to limit SARS-CoV-2, in similar fashion to those already reported (Dong et al., 2020; Elfiky, 2020; Gordon et al., 2020; Li and De Clercq, 2020; Wang et al., 2020); until one of these is proven to be beneficial in a clinical setting, all should be pursued as rapidly as possible.
Ivermectin has an established safety profile for human use (Gonzalez Canga et al., 2008; Jans et al., 2019; Buonfrate et al., 2019), and is FDA-approved for a number of parasitic infections (Gonzalez Canga et al., 2008; Buonfrate et al., 2019). Importantly, recent reviews and meta-analysis indicate that high dose ivermectin has comparable safety as the standard low-dose treatment, although there is not enough evidence to make conclusions about the safety profile in pregnancy (Navarro et al., 2020; Nicolas et al., 2020). The critical next step in further evaluation for possible benefit in COVID-19 patients will be to examine a multiple addition dosing regimen that mimics the current approved usage of ivermectin in humans. As noted, ivermectin was the focus of a recent phase III clinical trial in dengue patients in Thailand, in which a single daily dose was found to be safe but did not produce any clinical benefit. However, the investigators noted that an improved dosing regimen might be developed, based on pharmacokinetic data (Yamasmith et al., 2018). Although DENV is clearly very different to SARS-CoV-2, this trial design should inform future work going forward. Altogether the current report, combined with a known-safety profile, demonstrates that ivermectin is worthy of further consideration as a possible SARS-CoV-2 antiviral.
2. Methods
2.1. Cell culture, viral infection and drug treatment
Vero/hSLAM cells (Ono et al., 2001) were maintained in Earle's Minimum Essential Medium (EMEM) containing 7% Fetal Bovine Serum (FBS) (Bovogen Biologicals, Keilor East, AUS) 2 mM L-Glutamine, 1 mM Sodium pyruvate, 1500 mg/L sodium bicarbonate, 15 mM HEPES and 0.4 mg/ml geneticin at 37 °C, 5% CO2. Cells were seeded into 12-well tissue culture plates 24 h prior to infection with SARS-CoV-2 (Australia/VIC01/2020 isolate) at an MOI of 0.1 in infection media (as per maintenance media but containing only 2% FBS) for 2 h. Media containing inoculum was removed and replaced with 1 mL fresh media (2% FBS) containing Ivermectin at the indicated concentrations or DMSO alone and incubated as indicated for 0–3 days. At the appropriate timepoint, cell supernatant was collected and spun for 10 min at 6,000 g to remove debris and the supernatant transferred to fresh collection tubes. The cell monolayers were collected by scraping and resuspension into 1 mL fresh media (2% FBS). Toxicity controls were set up in parallel in every experiment on uninfected cells.
2.2. Generation of SARS-CoV-2 cDNA
RNA was extracted from 200 μL aliquots of sample supernatant or cell suspension using the QIAamp 96 Virus QIAcube HT Kit (Qiagen, Hilden, Germany) and eluted in 60 μl. Reverse transcription was performed using the BioLine SensiFAST cDNA kit (Bioline, London, United Kingdom), total reaction mixture (20 μl), containing 10 μL of RNA extract, 4 μl of 5x TransAmp buffer, 1 μl of Reverse Transcriptase and 5 μl of Nuclease free water. The reactions were incubated at 25 °C for 10 min, 42 °C for 15 min and 85 °C for 5 min.
2.3. Detection of SARS-CoV-2 using a TaqMan Real-time RT-PCR assay
TaqMan RT-PCR assay were performed using 2.5 μl cDNA, 10 μl Primer Design PrecisonPLUS qPCR Master Mix 1 μM Forward (5′- AAA TTC TAT GGT GGT TGG CAC AAC ATG TT-3′), 1 μM Reverse (5′- TAG GCA TAG CTC TRT CAC AYT T-3′) primers and 0.2 μM probe (5′-FAM- TGG GTT GGG ATT ATC-MGBNFQ-3′) targeting the BetaCoV RdRp (RNA-dependent RNA polymerase) gene or Forward (5′-ACA GGT ACG TTA ATA GTT AAT AGC GT -3′), 1 μM Reverse (5′-ATA TTG CAG CAG TAC GCA CAC A-3′) primers and 0.2 μM probe (5′-FAM-ACA CTA GCC ATC CTT ACT GCG CTT CG-286 NFQ-3′) targeting the BetaCoV E-gene (Corman et al., 2020). Real-time RT-PCR assays were performed on an Applied Biosystems ABI 7500 Fast real-time PCR machine (Applied Biosystems, Foster City, CA, USA) using cycling conditions of 95 °C for 2 min, 95 °C for 5 s, 60 °C for 24 s. SARS-CoV-2 cDNA (Ct~28) was used as a positive control. Calculated Ct values were converted to fold-reduction of treated samples compared to control using the ΔCt method (fold changed in viral RNA = 2^ΔCt) and expressed as % of DMSO alone sample. IC50 values were fitted using 3 parameter dose response curves in GraphPad prism.
Funding
This work was supported by a National Breast Cancer Foundation Fellowship, Australia (ECF-17-007) for KMW and an National Health and Medical Research Council (NHMRC), Australia Senior Prinicple Research Fellow (SPRF) (APP1103050) for DAJ.
References
- Buonfrate et al., 2019
- D. Buonfrate, et al.Multiple-dose versus single-dose ivermectin for Strongyloides stercoralis infection (Strong Treat 1 to 4): a multicentre, open-label, phase 3, randomised controlled superiority trialLancet Infect. Dis., 19 (11) (2019), pp. 1181-1190
- Caly et al., 2012
- L. Caly, K.M. Wagstaff, D.A. JansNuclear trafficking of proteins from RNA viruses: potential target for anti-virals?Antivir. Res., 95 (2012), pp. 202-206
- Corman et al., 2020
- V.M. Corman, et al.Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCREuro Surveill., 25 (3) (2020)
- Dong et al., 2020
- L. Dong, S. Hu, J. GaoDiscovering drugs to treat coronavirus disease 2019 (COVID-19)Drug Discov. Ther., 14 (1) (2020), pp. 58-60
- Elfiky, 2020
- A.A. ElfikyAnti-HCV, nucleotide inhibitors, repurposing against COVID-19Life Sci., 248 (2020), p. 117477
- Frieman et al., 2007
- M. Frieman, et al.Severe acute respiratory syndrome coronavirus ORF6 antagonizes STAT1 function by sequestering nuclear import factors on the rough endoplasmic reticulum/Golgi membraneJ. Virol., 81 (18) (2007), pp. 9812-9824
- Gonzalez Canga et al., 2008
- A. Gonzalez Canga, et al.The pharmacokinetics and interactions of ivermectin in humans--a mini-reviewAAPS J., 10 (1) (2008), pp. 42-46
- Gordon et al., 2020
- C.J. Gordon, et al.The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirusJ. Biol. Chem., 295 (15) (2020 Apr 10), pp. 4773-4779
- Gotz et al., 2016
- V. Gotz, et al.Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP importSci. Rep., 6 (2016), p. 23138
- Hiscox et al., 2001
- J.A. Hiscox, et al.The coronavirus infectious bronchitis virus nucleoprotein localizes to the nucleolusJ. Virol., 75 (1) (2001), pp. 506-512
- Jans et al., 2019
- D.A. Jans, A.J. Martin, K.M. WagstaffInhibitors of nuclear transportCurr. Opin. Cell Biol., 58 (2019), pp. 50-60
- Ketkar et al., 2019
- H. Ketkar, et al.Lack of efficacy of ivermectin for prevention of a lethal Zika virus infection in a murine systemDiagn. Microbiol. Infect. Dis., 95 (1) (2019), pp. 38-40
- Kosyna et al., 2015
- F.K. Kosyna, et al.The importin alpha/beta-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathwaysBiol. Chem., 396 (12) (2015), pp. 1357-1367
- Li and De Clercq, 2020
- G. Li, E. De ClercqTherapeutic options for the 2019 novel coronavirus (2019-nCoV)Nat. Rev. Drug Discov., 19 (3) (2020), pp. 149-150
- Lundberg et al., 2013
- L. Lundberg, et al.Nuclear import and export inhibitors alter capsid protein distribution in mammalian cells and reduce Venezuelan Equine Encephalitis Virus replicationAntivir. Res., 100 (3) (2013), pp. 662-672
- Lv et al., 2018
- C. Lv, et al.Ivermectin inhibits DNA polymerase UL42 of pseudorabies virus entrance into the nucleus and proliferation of the virus in vitro and vivoAntivir. Res., 159 (2018), pp. 55-62
- Mastrangelo et al., 2012
- E. Mastrangelo, et al.Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drugJ. Antimicrob. Chemother., 67 (8) (2012 Aug), pp. 1884-1894
- Navarro et al., 2020
- M. Navarro, et al.Safety of high-dose ivermectin: a systematic review and meta-analysisJ. Antimicrob. Chemother., 75 (4) (2020), pp. 827-834
- Nicolas et al., 2020
- P. Nicolas, et al.Safety of oral ivermectin during pregnancy: a systematic review and meta-analysisLancet Global Health, 8 (1) (2020), pp. e92-e100
- Ono et al., 2001
- N. Ono, et al.Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptorJ. Virol., 75 (9) (2001), pp. 4399-4401
- Rowland et al., 2005
- R.R. Rowland, et al.Intracellular localization of the severe acute respiratory syndrome coronavirus nucleocapsid protein: absence of nucleolar accumulation during infection and after expression as a recombinant protein in vero cellsJ. Virol., 79 (17) (2005), pp. 11507-11512
- Tay et al., 2013
- M.Y. Tay, et al.Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor IvermectinAntivir. Res., 99 (3) (2013), pp. 301-306
- Timani et al., 2005
- K.A. Timani, et al.Nuclear/nucleolar localization properties of C-terminal nucleocapsid protein of SARS coronavirusVirus Res., 114 (1–2) (2005), pp. 23-34
- van der Watt et al., 2016
- P.J. van der Watt, et al.Targeting the nuclear import receptor Kpnbeta1 as an anticancer therapeuticMol. Canc. Therapeut., 15 (4) (2016), pp. 560-573
- Wagstaff et al., 2011
- K.M. Wagstaff, et al.An AlphaScreen(R)-based assay for high-throughput screening for specific inhibitors of nuclear importJ. Biomol. Screen, 16 (2) (2011), pp. 192-200
- Wagstaff et al., 2012
- K.M. Wagstaff, et al.Ivermectin is a specific inhibitor of importin alpha/beta-mediated nuclear import able to inhibit replication of HIV-1 and dengue virusBiochem. J., 443 (3) (2012), pp. 851-856
- Wang et al., 2020
- M. Wang, et al.Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitroCell Res., 30 (3) (2020), pp. 269-271
- Wulan et al., 2015
- W.N. Wulan, et al.Nucleocytoplasmic transport of nucleocapsid proteins of enveloped RNA virusesFront. Microbiol., 6 (2015), p. 553
- Wurm et al., 2001
- T. Wurm, et al.Localization to the nucleolus is a common feature of coronavirus nucleoproteins, and the protein may disrupt host cell divisionJ. Virol., 75 (19) (2001), pp. 9345-9356
- Yamasmith et al., 2018
- E. Yamasmith, et al.Efficacy and safety of ivermectin against dengue infection: a phase III, randomized, double-blind, placebo-controlled trialHe 34th Annual Meeting the Royal College of Physicians of Thailand, Internal Medicine and One Health, Chonburi, Thailand (2018)
- Yang et al., 2020
- S.N.Y. Yang, et al.The broad spectrum antiviral ivermectin targets the host nuclear transport importin alpha/beta1 heterodimerAntivir. Res. (2020), p. 104760
The authors would like readers to be aware of the following letter issued by the FDA titled: “Do Not Use Ivermectin Intended for Animals as Treatment for COVID-19 in Humans” at https://www.fda.gov/animal-veterinary/product-safety-information/fda-letter-stakeholders-do-not-use-ivermectin-intended-animals-treatment-covid-19-humans.